By Devina Thiono
In 2019, around 1.8 million new cancer cases are expected in the U.S. 12,000 out of this number are children aged 1-14, with leukemia accounting for a third of children cancer cases. Leukemia is a cancer that affects the blood. The main targets of leukemia are white blood cells, whose job is to fight infection. People with leukemia produce abnormal white blood cells that can not function properly. Eventually, the leukemic cells can overtake normal cells and lead to signs and symptoms associated with leukemia, such as weight loss, fever, feeling tired all the time, bleeding or bruising easily, and bone pain.
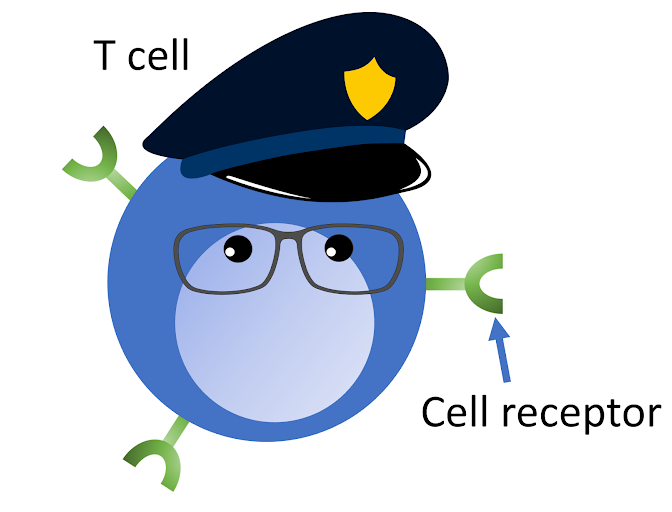
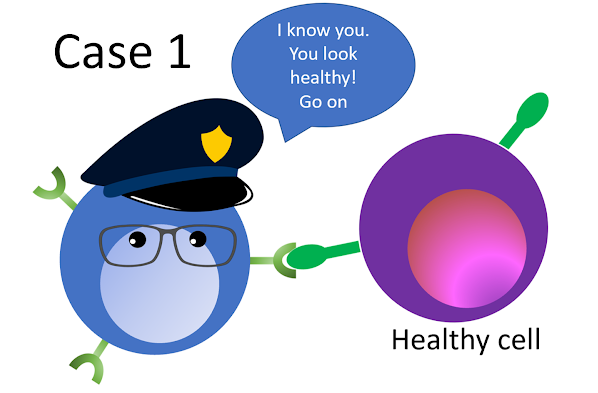
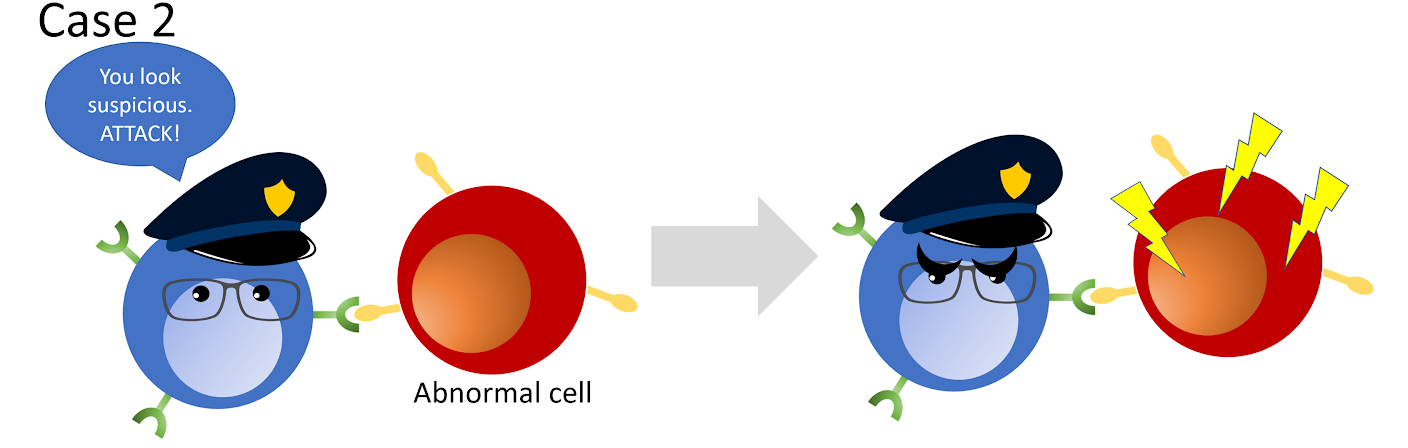
Even though our immune system is constantly protecting us from infection and disease, cancer has the ability to hide from the immune system. One type of immune cell that helps us to fight disease is the T cell. T cells usually go around and make sure the cells they pass by are healthy. The cell receptors on the surface of T cells allow them to sense whether the other cell is healthy or not. If T cells sense something is wrong with the other cell, it will attack the abnormal cell. However, cancer cells have gained the ability to escape T cell recognition. Consequently, many cancer patients do not know about the existence of cancer in their body until it has already developed and become more difficult to treat.
Scientists are trying to come up with new ways to fight cancer. One of them is through immunotherapy. Immunotherapy is a form of training for the immune system so it could recognize cancer cells better. The type of cancer and patient’s condition, such as their relative health status, determines the type of immunotherapy that is going to be used. There are many types of immunotherapies that use the immune system to fight cancer in different ways, one of them is CAR T-cells.
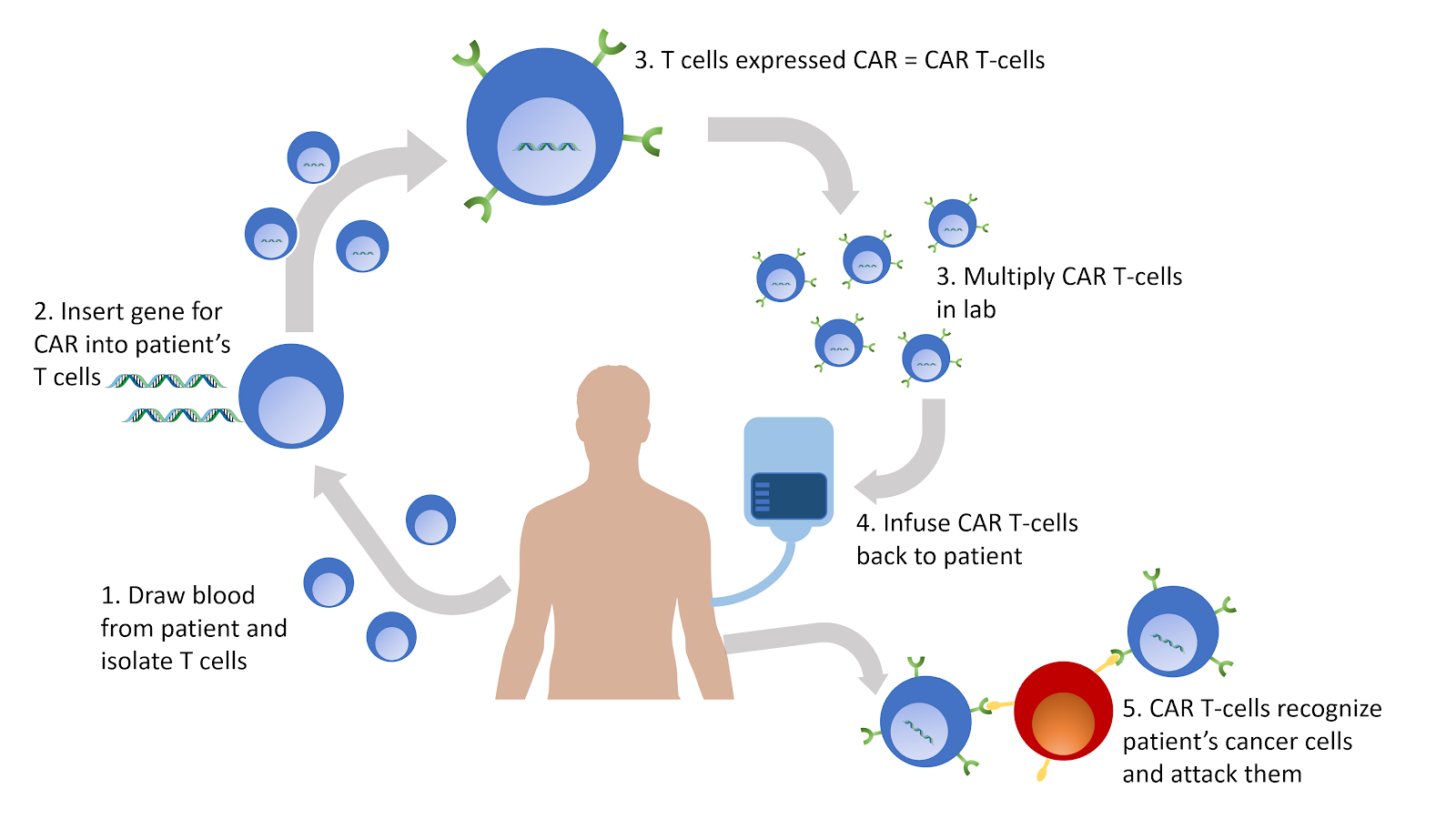
In CAR T-cells, scientists make T cell receptors that can specifically recognize the cancer cells that the patient has. This way, cancer cells have less chance to escape from CAR T-cells. The general procedure of the therapy is as followed:
- The patient’s blood is drawn and their T cells are collected.
- Artificial receptors, CAR, that are able to recognize cancer that the patient has will be added on the surface of the T cells.
- The modified CAR T-cells are multiplied in the lab.
- The CAR T-cells are infused back to the patient.
- Once inside the patient, the CAR T-cells will bind to the cancer cells that they recognize and attack them.
Currently, the FDA allows CAR T-cell therapy to be used on patients with adult B-cell non-Hodgkin’s lymphoma and childhood acute lymphoblastic leukemia who have had two unsuccessful standard treatments. However, clinical trials are being done to assess the possibility of using CAR T-cell therapy as the first or second option for cancer treatment in these patients.
As with other types of cancer treatments, CAR T-cell therapy does not always work on every patient. One of the reasons is that tumor cells constantly change, or mutate. This prevents CAR T-cells from recognizing tumor cells if the tumor cells have mutated inside the body during the time when CAR T-cells are still being developed in the lab. Scientists are working to design CAR T-cells that are able to recognize different parts of tumor cells. So, if one part of the tumor cell is mutated, CAR T-cells can still recognize other parts of the tumor cells.
Even though there is still room for improvement, this therapy has offered hope for people who had been diagnosed with cancer and given less than a year to live. Furthermore, CAR T-cells therapy is advantageous compared to conventional therapies because they can stay in the body for a long time. So, if the cancer returns, CAR T-cells are still able to take care of the cancer cells as long as the cancer cells have not mutated.
Check out past posts on immunotherapies that can be found in this blog here and here.
Edited by Elise Hickman and Rachel Battaglia