By Megan Frederick
Technique Name: Antibiotic Susceptibility Test (AKA Kirby-Bauer Test)
Fun Rating: 5/5
Difficulty Rating: 2/5
What is the general purpose? The antibiotic susceptibility test (also known as the Kirby-Bauer test) is used to determine the effectiveness of different antibiotics on certain types of bacteria. The main questions being asked are, “Is this type of bacteria susceptible or resistant to these antibiotics? Will the bacteria be able to grow, or will its growth be inhibited?”
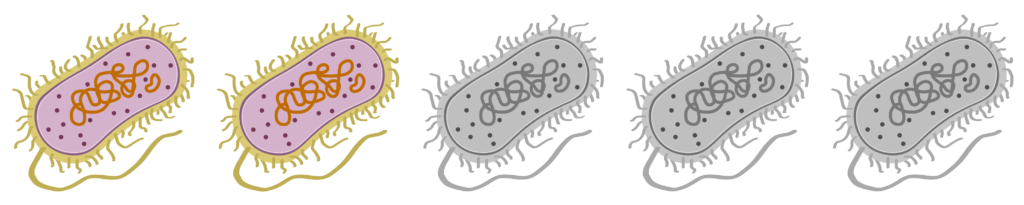
Why do we use it? Today, bacterial infections can be treated with a variety of antibiotics. When bacteria are sensitive or susceptible to a type of antibiotic, they are easily killed by the antibiotic. Unfortunately, some bacteria may become resistant to a type of antibiotic, allowing them to survive and overcome the effects of the antibiotic.
Scientists perform the antibiotic susceptibility test to determine which antibiotics a type of bacteria will be most susceptible to. This helps doctors determine which antibiotic to prescribe to patients infected with that particular bacteria. Prescribing an antibiotic that bacteria are very susceptible to helps ensure the treatment will work and also decreases the chances of bacteria developing resistance to that antibiotic.
How does it work? Many types of bacteria can be studied in the lab because they can grow on a nutrient-rich dish called an agar plate. Microscopic bacteria, meaning those you can’t normally see without a microscope, will become easily visible on the plate as they grow and replicate. Many types of bacteria can grow very well on regular agar, including bacteria that are isolated from patient samples such as blood, urine, open wounds, and mucus.
To perform the test, liquid containing the bacteria is evenly spread across the plate so that each bacterium (a single, microscopic bug) has plenty of room to grow. Next, small discs containing different antibiotics are added to the plate using tweezers. Finally, the plates are incubated at 37°C (which is equivalent to 98.6°F and right around your normal body temperature) for approximately 12 hours to allow the bacteria time to grow.
To determine if the type of bacteria is susceptible to an antibiotic, scientists will then look for a zone of inhibition around each antibiotic disc (Figure 1). These zones of inhibition occur when bacteria are unable to grow because of the presence of an antibiotic. This is because the antibiotic will diffuse away from the disc, creating a concentration gradient (Figure 2). The closer to the disc the bacteria try to grow, the higher the concentration of antibiotic. If the zone of inhibition around a disc is very large, meaning bacteria cannot grow very closely to the disc, this means that even small concentrations of the antibiotic are enough to inhibit or kill the bacteria. The larger the zone of inhibition, the more susceptible the bacteria is to that antibiotic.
Once a scientist determines the size of the zone of inhibition for each antibiotic, they can then recommend certain antibiotics to treat the infected patient. Ideally, an antibiotic will be selected that 1) will kill or inhibit bacterial growth at a relatively low concentration and 2) will not harm the patient receiving the antibiotic.
