by Macy Osborne-Frazier
Every year, around 23 million Americans visit the doctor to get treatment for a bacterial infection, so chances are you’ve been prescribed antibiotics at least once in your life. You might remember the doctor telling you to “make sure you don’t stop taking your medicine just because you’re feeling better.” That’s because you were likely prescribed antibiotics, a special type of drug designed to target and kill bacteria. Unlike many other drugs, antibiotics are normally prescribed to be taken for a set period of time, rather than just until you start to feel better. The reason antibiotics are prescribed this way is so you avoid developing antibiotic resistance. Antibiotic resistance happens when bacteria develop ways to avoid being killed by antibiotics. This can be a major problem, especially if bacteria become resistant to multiple different types of antibiotics because we can no longer cure people who are sick from bacterial infections. For people who are sick from bacteria that have acquired antibiotic resistance, this means they stay sicker for a longer period of time until doctors can find an antibiotic that the bacteria are susceptible to.
There are several ways that bacteria become resistant to antibiotics, but it is often due to overuse or misuse of antibiotics. Overuse happens when people are prescribed or take antibiotics when they don’t need them. One important thing to know about bacteria is that some bacteria are actually good for us, and we rely on the helpful bacteria that naturally live in our bodies to help us do things like break down food in our guts. If you take an antibiotic when you don’t really need it or take the wrong antibiotics, the drugs might instead attack harmless bacteria that live in our guts. To avoid being harmed by the unnecessary antibiotics, the harmless gut bacteria can mutate their DNA to become resistant to the antibiotics. This is great for our gut bacteria; however, these gut bacteria can then share the antibiotic resistance mutation they’ve acquired with harmful bacteria next time you get sick. Now the harmful bacteria are also resistant to the antibiotics you might be prescribed. In much the same way, when you misuse antibiotics by forgetting to take them when you should or stopping them early, the harmful bacteria now have time to mutate their DNA in a way that helps them become resistant to the antibiotic you were prescribed (Figure 1). Antibiotic resistance due to overuse and misuse of antibiotics is why it is so important to only take medicine when a doctor prescribes it and to take it in the way it was prescribed.
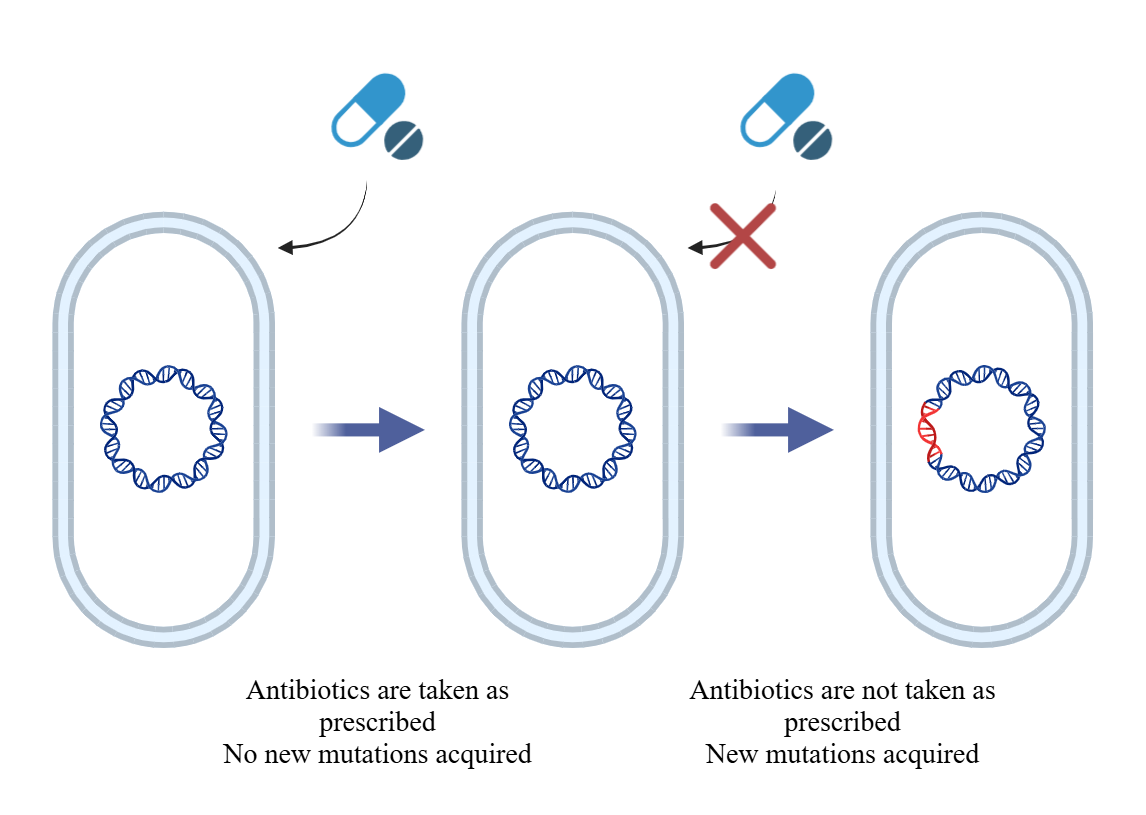
Figure 1. Illustration of bacterial cells acquiring new mutations (Created by author with BioRender.com)
Even though taking medicine when and how a doctor prescribes can help reduce antibiotic resistance, it can still arise when people take medicine exactly as prescribed. Although it is less common, it is important to understand how antibiotic resistance arises even when medicine is taken correctly so that researchers can develop ways to combat resistance. Antibiotic resistance naturally arises similarly to how it arises when people misuse antibiotics: through mutations in DNA. The DNA in bacteria naturally undergoes mutations all the time. When bacteria grow and divide, they must make copies of their DNA to share with the new bacteria that are formed. During the copying of DNA, accidents can happen that slightly alter, or mutate, the DNA, and if not caught by the cell, the mutations will become permanent. In addition, exposure to new environments or chemicals (like all the new environments or chemicals a bacterial cell will encounter in a human body) can cause mutations in bacterial DNA. Sometimes, the mutations that happen during DNA replication or exposure to new environments and chemicals result in mutations that code for antibiotic resistance
The other main way that people become infected with antibiotic resistant bacteria is through the spread of germs. Antibiotic resistant bacterial infections are spread the exact same way normal bacterial infections are. This is why it is so important to practice healthy hygiene habits like washing your hands. We don’t want to spread or become sick with normal bacterial infections, but we really don’t want to further the spread of antibiotic resistant bacterial infections that are much harder and more expensive to cure.
Although there are several ways that antibiotic resistant bacterial infections develop and are spread, biomedical scientists are always studying new bacteria and working to develop new antibiotics to help fight the bacteria that have developed resistance to common antibiotics. This cold and flu season make sure to be mindful of how antibiotic resistant bacterial infections begin and are spread (Figure 2). If a doctor prescribes you antibiotics, make sure you aren’t resistant to your medicine unless you want the bacteria to become resistant too!
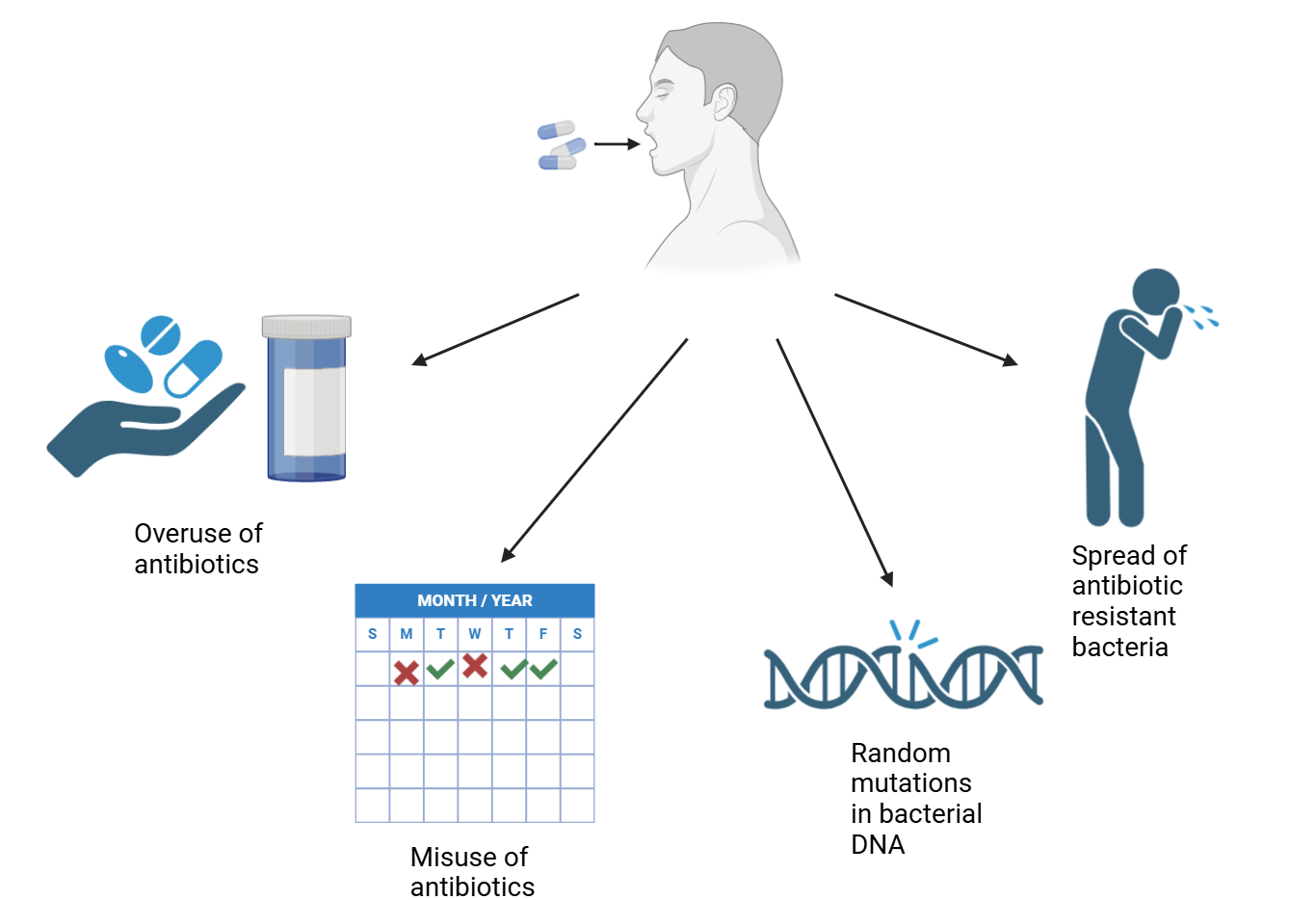
Figure 2. Illustration of how antibiotic resistant bacteria develop and are spread (Created by author with BioRender.com)
