By Yitong Li
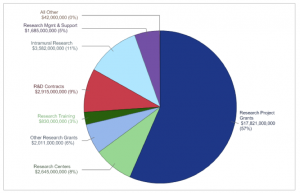
One of the biggest funding agencies in the United States, the National Institutes of Health (NIH) spends about $32 billion every year to support scientific research that contributes to the wellbeing of Americans. If you consider the annual household income in US (~$55k), the NIH budget is equivalent to the total annual income of 580,000 families. However, despite this huge financial input and the effort of 300,000 researchers, over half a million patients still die from cancer each year, over 600,000 people die of heart disease, and much more if we count every single fatal illness. So has the NIH sponsored biomedical research actually contributed to our health?
The simple answer is yes, but there is more than just the figures during this “bench-to-bedside” process. While the news reports each day that a group of scientists have identified a potential therapeutic target for a specific cancer, heart attack, or some type of liver disease, only a few of these scientific discoveries eventually stumble their way to the clinic for treating patients. For instance, only 8% of animal studies on cancer therapies have been successfully translated to clinical trials where human patients test the new drugs. With the huge financial and time input, why is the progress of translating scientific discoveries from the bench to clinic still inefficient?
To understand this issue, let’s start by taking a look at how science is conducted in the lab. In general, scientists use both in vitro (in a test tube or culture dishes, outside of a living organism) and in vivo (in a living organism) systems to study a specific question. For example, cancer researchers may analyze what’s causing tumors to grow so fast by growing cancer cells that were isolated from a patient and grown in a dish – the in vitro system. They may also use mice that have mutations to grow tumors – the in vivo system. Both systems have pros and cons. For instance, most cultured cells are easy to manipulate for various experiments, but cells growing on a plastic dish behave differently than when they are in the human body. Just like us, cells have their own “social” structures and different types of cells work together to keep our body healthy. These complex interactions are hard to replicate outside of the body, making the discoveries from in vitro studies oversimplified. On the other hand, mice provide the advantage of studying cells in their natural environment where all the complicated interactions are maintained. Nevertheless, genetic, molecular, and physiologic differences between mice and humans still limit the application of these in vivo discoveries to human patients.
If mice are so different from us, why don’t scientists use animals that are more similar, such as primates? The answers fall into three categories: cost, efficiency, and ethics. Ethics is a complex issue, so I will only focus on cost and efficiency here. Caring for larger animals requires more money and effort. Mouse studies are already costly, but when it comes to studies using rabbits, dogs, and primates, the increased cost in maintaining these animals can be a deal breaker. Larger mammals also have longer gestation periods and life spans, thus slowing down the rate of experiments. Due to the high costs associated with conducting studies in these animals, only a small portion of the chemical compounds identified from mouse studies are selected for testing in larger mammals. The few drugs that are successful will move on to clinical trials in humans, which can take another four years at least, before the good candidates are approved by the Food and Drug Administration (FDA) to treat patients. The lengthy and expensive process of obtaining FDA approval to finally bring the scientific discoveries to patients, which is hard to obtain federal support on, severely discourages, if not excludes, a lot of scientists from translating their discoveries.
With that being said, why do I still believe that the NIH sponsored biomedical research has contributed to our health? Bench research is nevertheless the foundation of everything. Without all the findings from cell culture and mouse studies, there would be no targets or candidates to start with. Many scientists are well aware of the lack of clinical translation and have contributed to changing the status quo, such as generating a hybrid animal model where specific human cells are grown inside of the mice. Their effort in bridging the gap between bench and bedside light up the hope that more scientific discoveries made at the bench will be applied to patients and help them obtain a better quality of life.
Edited by Sam Stadmiller and Sarah Marks