By Carolina A. Herrera
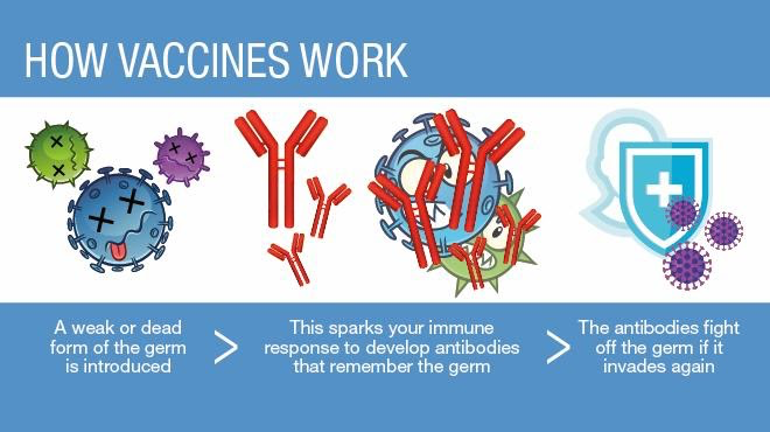
Vaccines train your immune system to fight against harmful invading pathogens, which are microorganisms (bacteria, viruses, fungi and parasites) that can cause disease. Vaccines contain dead or weakened pathogens, or distinctive pieces of a pathogen such as proteins or polysaccharides (sugars) that activate the immune system.
The immune system is a network of cells, tissues and organs that protects your body against infection. The immune system is made up of various white blood cells such as dendritic cells, monocytes/macrophages, T cells and B cells which work together to combat infectious microorganisms. Immune cells such as dendritic cells and monocytes are able to detect pathogens and ingest, or eat, them via a process called phagocytosis. When these cells ingest pathogens, they break them down into fragments called antigens, and display them on the cell surface. Antigens on the cell surface act as a tag and are recognized by T cells. T cells then become activated and proliferate into helper T cells and cytotoxic T cells. Activated helper T cells play a major role in helping B cells produce antibodies, proteins that help with the detection and destruction of pathogens. Once activated, B cells multiply and produce antibodies specific to the pathogen. Antibodies tag infected cells so that cytotoxic T cells can locate and kill these cells.
Once this process has been initiated for a pathogen, it usually happens much more quickly and robustly the next time your body sees that same pathogen. Vaccines mimic a weak infection that triggers an immune response so that the immune system will be prepared for a future infection–eliminating the need for you to actually catch the disease first before developing immunity. Vaccines also activate memory B-cells which can survive for decades in the body and repeatedly generate immune responses if you come into contact with the pathogen in the future!
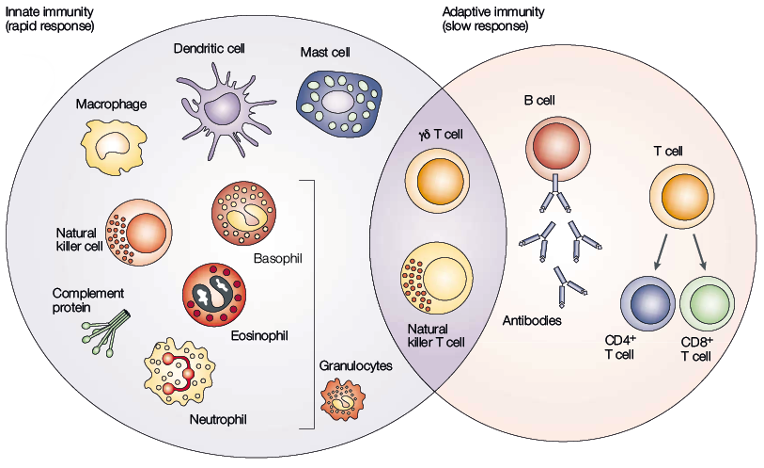
Source: Dranoff G. Nat Rev Cancer 2004;4:11-22
Over the course of history, vaccines have effectively proven to be beneficial for public health. Vaccines have eradicated smallpox and nearly eliminated polio virus worldwide. In addition, the number of people infected with measles, diphtheria, and whooping cough is at an all-time low according to the Centers for Disease Control and Prevention (CDC).
New pathogens emerge throughout time, so scientists keep developing new vaccines. The pathogen that is currently a priority for vaccine development is the SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2) which causes coronavirus disease-19 (COVID-19). Scientists have been working quickly to develop and test a vaccine for COVID-19. Developing effective vaccines requires years of research and rigorous safety measures before the vaccine is administered to the public. Although vaccines take time to produce, COVID-19 vaccines are going through required safety and efficacy tests at the fastest rate in history. Vaccine trials for COVID-19 are predicted to yield a safe FDA-approved vaccine by late this year or early next year according to the CDC.
Mayo Clinic
As of September 30, 2020, there are 11 vaccines in phase 3 clinical trials, which are large-scale tests that evaluate the efficacy and safety of the vaccine. Phase 3 clinical trials are the second to last phase before a drug or vaccine is available to the public. The leading companies in the United States carrying out phase 3 clinical trials for the coronavirus vaccine are Moderna and Pfizer. Moderna is currently enrolling 30,000 healthy individuals and Pfizer is enrolling 43,000. The vaccines in development at both companies are mRNA vaccines. Using the SARS-CoV-2 virus genome, scientists identified the sequence for the coronavirus spike protein, the protein the virus uses to enter host cells. The instructions for making the spike protein are encoded into a molecule called mRNA, which can be directly administered to patients as a vaccine. The mRNA instructs immune cells to make copies of the spike protein so the body can carry out an immune response and produce antibodies against the virus.
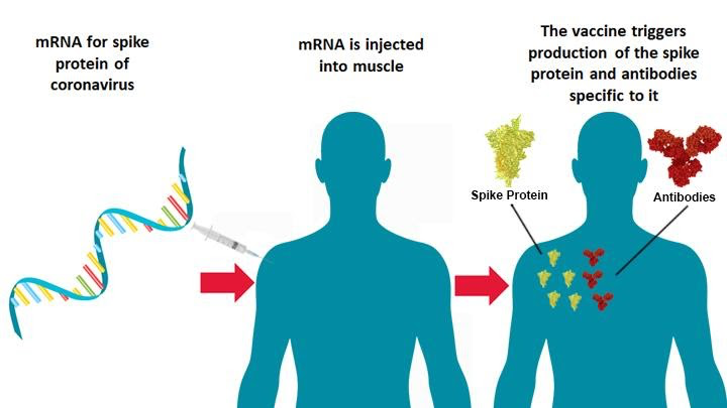
National Institutes of Health
Vaccines have proven effective in protecting individuals globally from pandemics. Scientists are conducting research to improve vaccines every day to prevent disease and stop pathogens in their tracks. Stay tuned!
