by Devina Thiono
Image was generated bu author using Biorender.com.
A vaccine is an effective way to train our immune system to handle an infection caused by pathogens (e.g. virus, bacteria, parasite) before the real infection hits us. There are many types of vaccines, with the mRNA (short for messenger ribonucleic acid) vaccine being the newest one that was approved for use in humans. It usually takes, at a minimum, around 5 years for a new vaccine to be developed. However, the SARS-CoV-2 mRNA vaccine was authorized for emergency use in the United States in less than a year after the pandemic started, and given full FDA approval in less than two years. Many people were puzzled as to why the SARS-CoV-2 mRNA vaccines could be developed so quickly. However, this technology is not new. In fact, scientists have been looking into the idea of delivering lab-generated mRNA into animals as early as the 1990s. So, the real question is why does it take so long to develop a mRNA vaccine?
Let’s go back up a step to understand what mRNA is and what it does. You can envision mRNA as a long sequence of 4 different letters that makes up a code. This code is translated by our cells to make a protein. In the case of the Pfizer/BioNTech and Moderna COVID19 mRNA vaccine, they include the code for the spike protein of SARS-CoV-2 in the mRNA sequence (Fig. 1). Once this mRNA is delivered into our cells, our cells will then read this code and produce their own SARS-CoV-2 spike protein. This protein will then be used to train our immune cells to develop a defense against the real SARS-CoV-2 (Fig. 2). For this whole process to work, the mRNA must find a way to get into our cells. This was a challenge that scientists have been trying to solve for years.
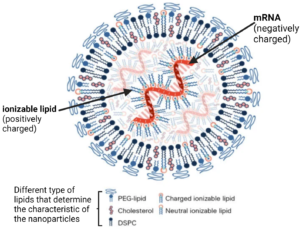
One of the major challenges of delivering external mRNA into our body is that free-floating mRNA gets broken down quickly; thus, stopping it from delivering its message into the cells. Scientists were looking for ways to overcome this challenge. One of the solutions, which is used in the current COVID19 mRNA vaccines, is to carry the mRNA inside bubbles of fat-like particles, called lipid nanoparticles (Fig. 3). These lipid nanoparticles protect the mRNA from being broken down, and deliver it safely to our cells. Furthermore, the addition of polyethylene glycol (PEG)-lipid on the surface of the nanoparticles, and ionizable lipids could make these lipid nanoparticles last longer in the body and reduce toxicity.
Another major challenge was to reduce the body’s defense mechanisms upon detecting the external mRNA. Our cells are equipped with many sensors that are tasked with identifying foreign materials as danger signals. Unfortunately, this includes mRNA vaccines. In 2005, a study led by Katalin Karikó found a way to overcome this, which is used in the current COVID19 mRNA vaccines. mRNA codes are made up of a combination of 4 different chemical bases: adenine (A), cytosine (C), guanine (G), and uracil (U). Karikó and team found that changing the U into pseudouridine (Ψ) helps to “dampen” our body’s danger signal upon seeing this external mRNA. Consequently, this modification prevents the mRNA from being attacked and destroyed by our immune cells, and allows the message it encodes to be safely delivered into our cells.
As you can see, the different technologies that make the current COVID19 mRNA vaccines were developed a long time ago even before the SARS-CoV-2 pandemic. In fact, in the past mRNA delivery platforms have been studied for cancer vaccines, and other infectious diseases, such as HIV, Zika, rabies and influenza. One of the beauties of mRNA delivery platforms is the fact that you can change the mRNA coding sequence of one protein with another protein of interest. Thus, once we have all the right components to deliver this mRNA into the right cells promptly and safely, the platform can be used for a myriad of other purposes!
