by Siena Mantooth
I lived outside as a child, and naturally, I got fairly dirty. My hands and feet would be full of mud, splinters, and grime more often than not. Thankfully, my mom had taught me good hygienic practices, and I washed most of the outside particles down the drain. However, I occasionally found a splinter embedded under my skin, and the longer it stayed there, the more redness and swelling appeared at that spot. My dad sterilized a sewing needle by sticking it into a lit match, and he used it to delicately pop that tiny piece of wood out from under my skin. Oftentimes, pus surrounded the splinter, and we drained the pool of opaque goo, leaving my skin smooth and bump-free.

Little did I know then, that the pus was protecting me from foreign bacteria and viruses. Every person has an immune system protecting them from outside invaders. Three lines of defense protect the body: physical and chemical barriers, the non-specific/innate immune system, and the specific/adaptive immune system. The first line is natural barriers, which include the skin (as seen in the image below) and mucus membranes, like those inside your nose. These anatomical barriers allow you to walk outside without your immune system going into overdrive. However, objects like splinters can breach the skin, causing the immune system to activate a response called the foreign body reaction (FBR) that includes the activation of the innate and adaptive immune systems.

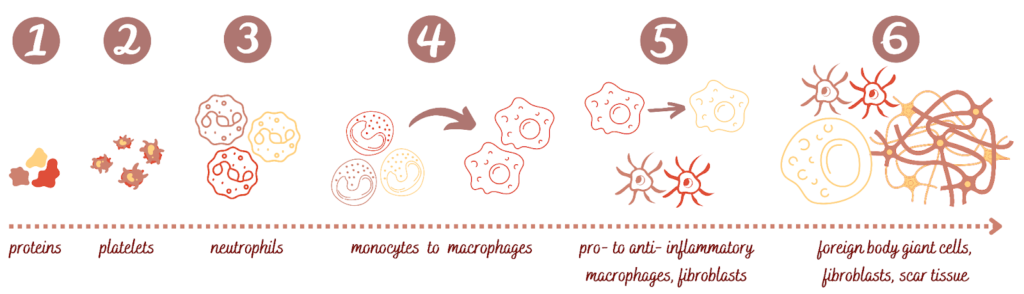
The FBR follows a natural progression of events (see the diagram below):
- First, within seconds of an object being implanted under the skin, blood proteins adhere to the surface of the material.
- Platelets, cells that circulate in our blood, then try to form a clot around the material, and proteins that encourage cell adhesion also stick to the surface.
- Neutrophils, a type of immune cell that is predominantly found in pus, swoop in to destroy the material by eating it (a process called “phagocytosis”). They also release proteins called chemokines to attract other immune cells.
- However, if the neutrophils cannot destroy the object, another immune cell called a monocyte comes to the rescue. At this point, the neutrophils either die or flee the premises. The monocytes change into macrophages, which work tirelessly to destroy the object through releasing factors like chemical compounds, enzymes, and acid and trying again to eat it.
- As early as five days after the material has been implanted, if the material still cannot be removed, the macrophages become frustrated. They change from pro-inflammatory to anti-inflammatory and now try to rebuild a wall around the material, with the help of cells called fibroblasts. This transition allows the body to repair itself rather than continuing to attack the foreign object.
- Macrophages sticking to the material fuse together to form foreign body giant cells (FBGCs), which cause long-lasting or chronic inflammation.
At this point, a whole host of other immune cells are present, FBGCs are attached to the material, and the fibroblasts and other cells have built a wall of scar tissue around the object. Since the material could not be removed, it has now been encapsulated and hidden from the body about 3 to 4 weeks after the initial implantation.
Normally, I caught my splinter at the neutrophil or pus stage. However, had I left it in my skin for a month, I would have had a wall of scar tissue surrounding it as a result of a prolonged FBR. Most of the time, we want our bodies to react and protect against foreign unwanted objects. However, the FBR is a major reason that so many biomaterial devices fail after implantation in an individual’s body. Implants, biosensors, and other devices have to address the FBR in order to work appropriately, so understanding the immune response can help biomedical engineers and scientists create usable systems to put into the body. The FBR protects us, but we need to work with it to continue to develop life-saving medical technology.
