by Garima Singh
Most of us know someone with asthma who brings their inhaler with them everywhere they go, and for good reason! Asthma is a chronic inflammatory disease of the airways that makes it difficult to breathe. In mild cases, it disrupts daily activities, but can be life-threatening in more severe cases. This condition is fairly common, affecting almost 26 million people in the United States, 7 million of whom are children. Although the exact cause of asthma is not known, various genetic and environmental factors play an important role in how this condition develops. So how exactly does asthma affect one’s ability to breath and how do inhalers help?
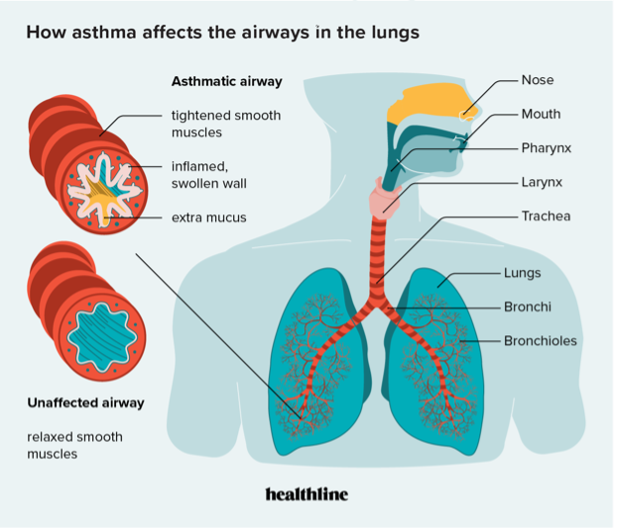
An asthma attack occurs when a person is exposed to a trigger like pollen, smoke, dust, or household chemicals. The exposure to these particles causes inflammation that leads to the narrowing of airways in the lungs. This happens when the smooth muscles surrounding the airways swell and produce excessive mucus, reducing the size of the airways [Figure 1]. The narrowing of the bronchi (bronchoconstriction) reduces the flow of air in and out of the lungs making it harder to breathe. This results in symptoms one normally associates with asthma, such as wheezing, shortness of breath, chest tightness, and coughing. A more in-depth look into the pathophysiology of asthma can be found here. Different triggers can cause different kinds of asthma which include:
- Allergic asthma
- Cough-variant asthma
- Exercise-induced asthma
- Nighttime asthma
- Steroid-resistant asthma
- Occupational asthma
It is important to understand the triggers in order to determine what kind of inhaler would be most suited for treating symptoms.
Inhalers: Quick fixes and long-term solutions
Inhalers, also known as bronchodilators, have two goals: to open up the airways (bronchodilation) and to decrease inflammation, allowing for increased airflow. There are three basic types of inhalers that deliver medications:
- Metered-dose inhaler (or MDI) – Uses pressure to push the medication out of the inhaler.
- Nebulizers – Uses air or oxygen to deliver a mist of the medication through a tube or mask that fits over your nose and mouth.
- Dry powder inhalers (or DPIs) – Deliver medication directly, require a strong and fast inhalation
Asthma medication contained in these inhalers falls under “reliever,” “controller,” “preventer,” or combination drug therapy. Short-acting bronchodilators are “reliever,” “quick-relief,” or “rescue” inhalers containing β2-adrenergic receptor agonists. β2 receptors bind to adrenaline, the “fight-or-flight” hormone which the body releases in times of stress. Adrenaline decreases blood pressure by dilating the blood vessels which causes the smooth muscles surrounding the airways to relax. This allows the airways to open up, relieving the acute symptoms of asthma. Short-acting bronchodilators are therefore most useful for sudden attacks, as in the case of allergic and exercise induced asthma. This type of medication works rapidly but is short-acting and thus is usually used only as needed. Albuterol is the most well known and widely used drug in this category.
Unlike short-acting β-agonists, long-acting β-agonists or “controllers” do not work on muscle inflammation directly. Instead, they target airways to allow for greater passage of air. They are usually taken with an inhaled steroid which is an anti-inflammatory medication. This “preventer,” when taken twice a day helps decrease airway inflammation long-term. Thus long-acting β-agonists provide control to reduce asthma attacks, not quick relief. These medications take time to work, and therefore require daily use, and can’t be used as needed.
Asthma is a serious condition which can be difficult to manage given its many triggers. We should thus be mindful of the people around us living with asthma so as to not trigger their symptoms by our actions while also being able to recognize signs of distress to help if needed.
If you’re in distress or see someone in need of assistance, inform a teacher or nurse and follow the steps below:
