by Tiffany Ko
It’s hard to believe that four years have already passed since the World Health Organization (WHO) announced Coronavirus Disease 2019 (COVID-19) as a global pandemic. Since then, scientists have developed vaccines that have saved millions of lives. Although vaccines have reduced the prevalence of COVID-19, no vaccine can be 100% effective, and people still develop COVID. An estimated 10-20% of people infected by SARS-CoV-2, the virus that causes COVID-19, have developed Long COVID, otherwise known as Post-acute sequelae of COVID (PASC) or Post-COVID Conditions (PCC).
Long COVID is defined as symptoms that either continue from or develop after an initial SARS-CoV-2 infection and last for at least two months. To be considered Long COVID, there must be no other explanation for the symptoms. The list of symptoms is long (pun intended), including fatigue, brain fog, headaches, gastrointestinal symptoms, rapid or pounding heartbeat, loss or change in smell or taste, cough, chest pain, and sleep problems. Of course, there are more symptoms than just the ones listed here. Each person may even have a different combination of symptoms. For some people, their symptoms are mild. For others, their symptoms keep them from their normal daily activities: going to school, walking upstairs, or cooking dinner can be extremely difficult for some with Long COVID.
Fortunately, evidence shows that vaccination against COVID-19 reduces the risk of people developing Long COVID. And although anyone who has been infected with SARS-CoV-2 could develop Long COVID, it occurs most often in people who have had severe COVID-19. It can take a long time to receive a Long COVID diagnosis because doctors must first exclude any other possible causes. Doctors may use a variety of tests, like physical exams, blood pressure and heart rate measurements, cognitive tests, or chest X-rays, depending on the patient’s symptoms, to determine if a patient has Long COVID. Since the symptoms include a broad range of organs, there is currently no one-size-fits-all treatment for Long COVID. Depending on their symptoms, a patient might work with a team of doctors with different specialties to develop a treatment plan together.
What causes people to develop long COVID? Researchers are still working on finding the answer, but there are a few possibilities backed up by evidence. One theory is that a little of the SARS-CoV-2 virus remains in an organ (or several organs) leading to an inflammatory response. Another theory is that after SARS-CoV-2 infection, there is reactivation of different viruses from past infections that have been dormant or inactive in a person’s body. For example, the Epstein-Barr virus (a virus that can cause mono) can remain in the body in an inactive state and could be reactivated by a SARS-CoV-2 infection. Some research also suggests that the inflammation caused by SARS-CoV-2 infection leads the body to overreact to its own cells in an autoimmune response. This is when the immune system targets and attacks the body’s own healthy tissues. A final theory is that SARS-CoV-2 infection leads to organ damage which could cause the symptoms of Long COVID. Since Long COVID has such a complicated and long list of symptoms, it is possible that different symptoms have different causes. To add to the complexity, it is also dependent on every person’s unique health and history.
The COVID-19 pandemic changed the world in many significant ways. For some people, COVID-19 has changed their whole lives because of chronic symptoms. Just as we saw the scientific and medical community leverage their effort into the development of the vaccine, we can hope that future research will lead to the development of treatments for Long COVID.
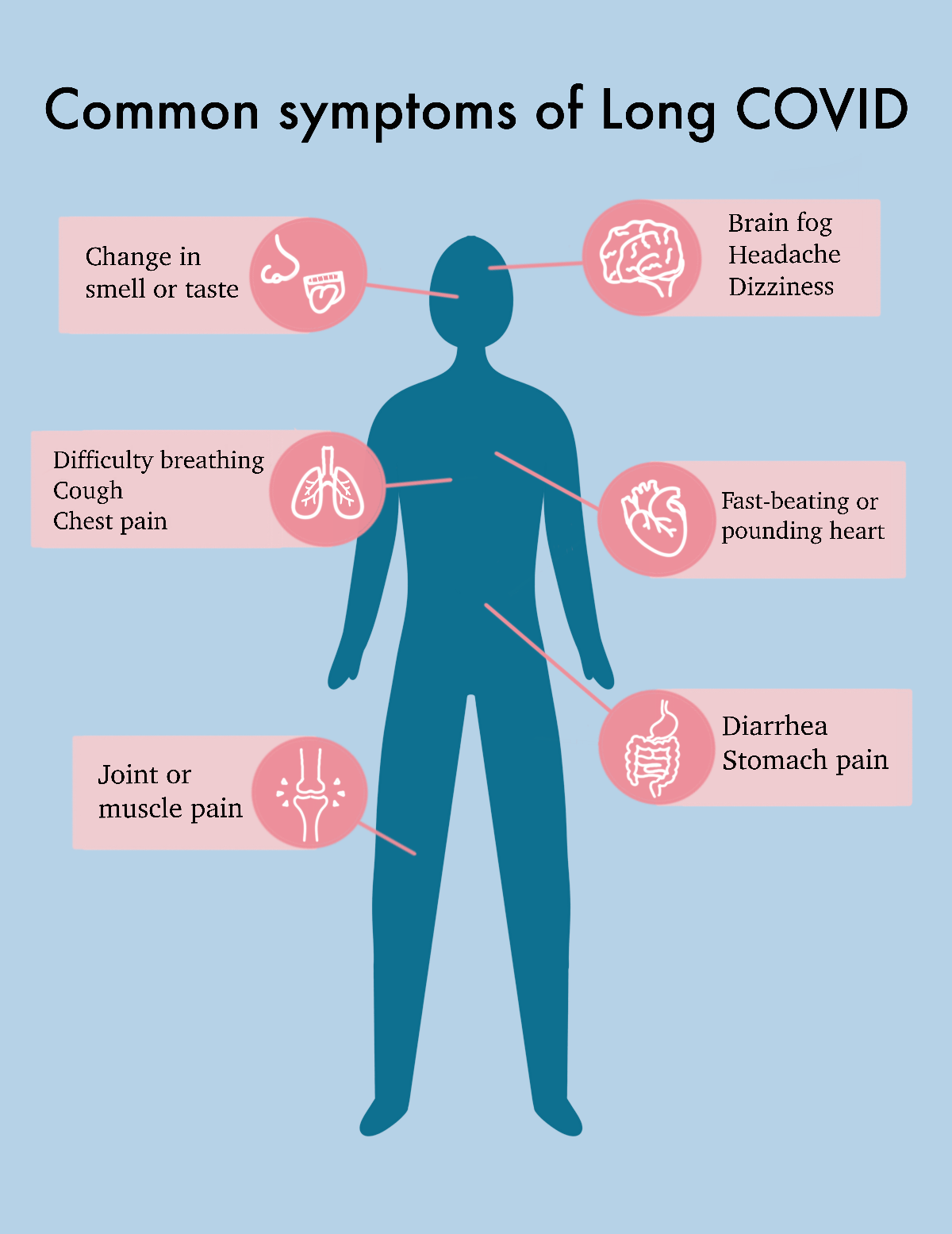
Common symptoms of Long COVID provided by the Center for Disease Control, illustrated by Tiffany Ko
