by Marco Gontijo
Tuberculosis (TB) has claimed more lives than any other infectious disease in the history of humanity, with estimates suggesting it has caused over a billion deaths in the last 200 years. TB isn’t just an ancient disease—it’s a clever one. Caused by the bacterium Mycobacterium tuberculosis (Mtb), TB doesn’t always cause illness right away. In fact, most people infected with TB don’t even know it. The bacteria have a remarkable trick: they can hide inside your body for years, even decades.
When Mtb cells enter the lungs, the immune system doesn’t always destroy them. Instead, immune cells called macrophages rush to the scene to contain the invader. These cells—and many other types of immune cells—form a tight cluster around the bacteria, creating a granuloma (Figure 1). The granuloma involves both innate (quick, front-line responders) and adaptive (specialized cells recruited later) immune cells. You can picture it like a biological fortress: the immune system builds a wall around the bacteria, trapping them inside and cutting off their resources.
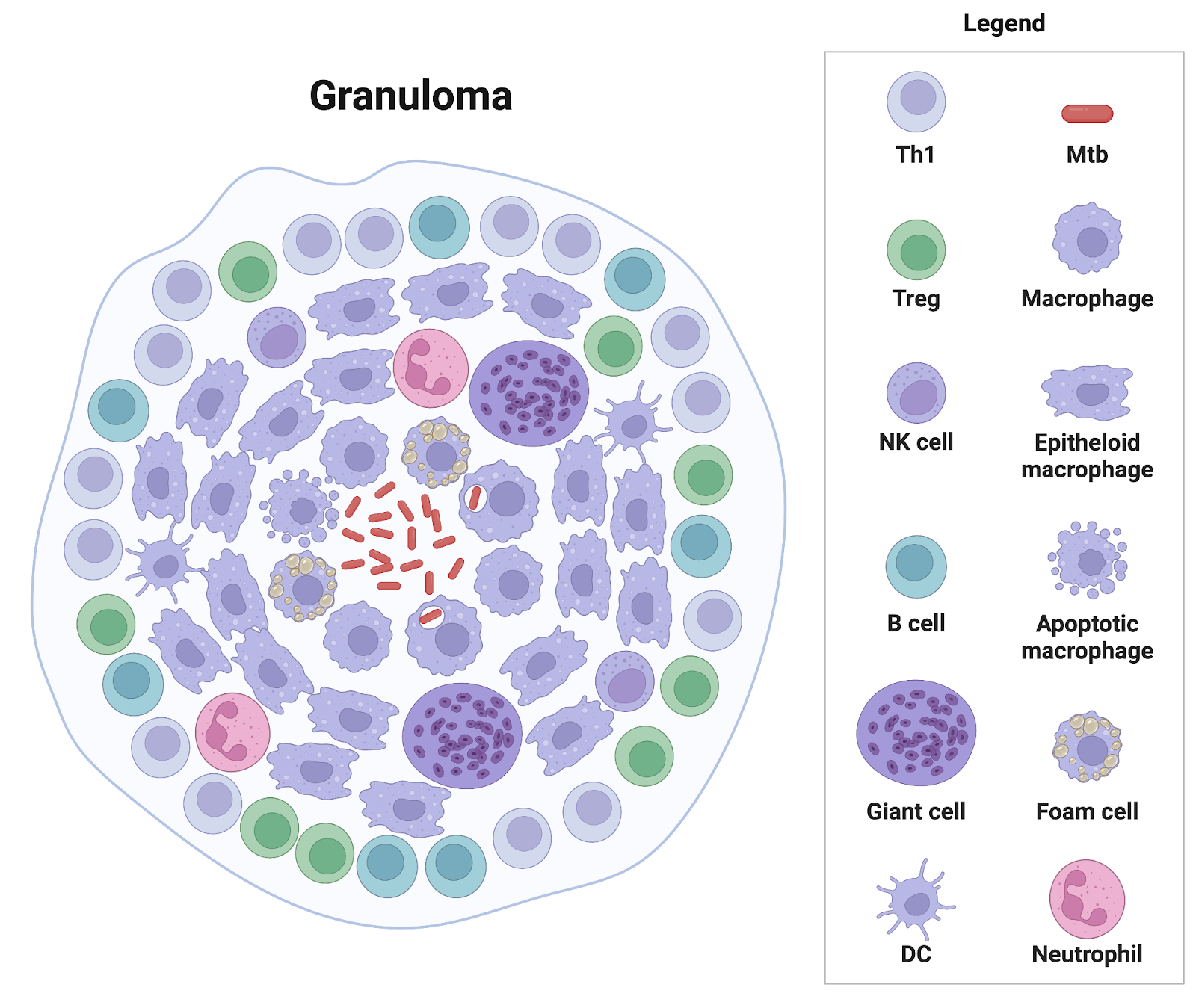
Figure 1. Structure of a tuberculosis granuloma. The image shows immune cells forming a layered structure to contain Mtb. Macrophages and other cells surround the bacteria to limit its spread, forming a granuloma. Image created in BioRender. Lab, S. (2025) https://BioRender.com/a92tnbr.
What is a granuloma?
A granuloma (Figure 1) is the body’s way of building a quarantine zone. When immune cells detect Mtb cells, they can’t destroy them; rather, they surround and trap them in a tight cluster. Think of it like a microscopic fortress made of immune cells. This helps prevent the infection from spreading but doesn’t always kill the bacteria. Instead, the Mtb cells go dormant inside the granuloma, hiding from the immune system and most antibiotics.
Inside this granuloma, TB goes into a kind of sleep mode, slowing its metabolism and becoming incredibly hard to kill. This state is called subclinical TB infection. People with subclinical TB don’t feel sick and can’t spread the disease—but the bacteria are still there, biding their time.
While tuberculosis is a classic example, granulomas can form in response to various infections and inflammatory diseases.
Is the Granuloma a Double-Edged Sword?
Yes—and that’s what makes TB so tricky. On one hand, granulomas are helpful because they wall off the bacteria, stopping the infection from spreading. On the other hand, they also create a safe space for Mtb to survive, hidden from the immune system and most antibiotics. This means the bacteria can stay dormant for years—and potentially reactivate later, significantly if the person’s immune system weakens. So while the granuloma is intended to protect us, it also helps the bacteria persist.
What Causes Subclinical TB to Reactivate?
Subclinical TB, often called “latent TB”, can quietly sit in the body for years without causing symptoms—but it doesn’t always stay that way. If the immune system weakens, the balance shifts. The bacteria inside the granulomas can “wake up” and start multiplying again, leading to active TB disease. Reactivation can be triggered by things like HIV infection, cancer treatments, aging, malnutrition, or chronic illnesses such as diabetes. That’s why people with weakened immunity are at higher risk and often need preventive treatment, even if their TB is dormant.
All of this is why TB is so difficult to eliminate. It doesn’t just infect—it hides, waits, and strikes when the body is most vulnerable.
